Dysmorphia (pronounced dis-mor-fiah)
(1) In clinical anatomy, characterized by
anatomical malformation.
(2) In general medicine, having or
exhibiting an anatomical malformation.
(3) In psychology and psychiatry, the
perception of anatomical malformation; any of various psychological disorders
whose sufferers believe that their body is wrong or inadequate, such as
anorexia, bulimia, and muscle dysmorphia (bigorexia).
(4) As Dismorphia astyocha, a butterfly in
the family Pieridae, found in both Argentina & Brazil.
From Ancient Greek δυσμορφίᾱ (dusmorphíā) (misshapenness, ugliness),
the construct being δυσ- (dus-) (hard,
difficult, bad) + μορφή (morphḗ) (shape,
form) + -ίᾱ (-íā). The prefix dys- was from the New Latin dys-,
from Ancient Greek δυσ- (dus-), (hard,
difficult, bad”) and was used to convey the idea of being difficult, impaired,
abnormal, or bad. Morph was a back-formation
from morpheme & morphism, attested since the 1950s, from the Ancient Greek
μορφή (morphḗ) (shape,
form) and related to the German Morph,
from Morphem (although dating only
from the 1940s). It’s probably now most
familiar in (1) formal grammar & linguistics as a physical form
representing some morpheme in language (it exists as a recurrent distinctive
sound or sequence of sounds), (2) in linguistics as an allomorph (one of a set
of realizations that a morpheme can have in different contexts) and (3) in
digital image processing where shapes are changed from one form to another with
the use of specialized software, a popular type being that which wholly or
(especially) partially blends two images.
The plural is dysmorphias and, in clinical use, the synonym is
dysmorphosis.
The word dysmorphia first appeared in the Histories of the Greek historian
Herodotus (circa 484–circa 425 BC) when he referred to the myth of the “ugliest girl in Sparta”. Herodotus, even in his lifetime, was
criticized for making an insufficient distinction between legend and historical
fact but the veracity of much of his work, subject to forensic analysis by
modern archeologists and archivists, has been established. The story of the “ugliest girl in Sparta”
however, Herodotus acknowledges as “a magical myth” in which a baby girl, born
in Sparta, was terribly disfigured (which he described as dysmorphia (meaning “misshapenness” or “ugliness”). Fortunately, she was from a well-connected
family and her nanny suggested taking her to the shrine of Helen of Troy on hilltop
of Therapne, and there pray for a cure. There
the nurse sat with the baby and while praying before the agalma (a carved image of Helen), from nowhere a apparition of
Helen appeared and smiling, laid her hand upon the child’s head. As the years passed, the disfigured infant would
grow to become the most beautiful girl in the kingdom.
Body Dysmorphic Disorder
Body dysmorphic disorder (BDD) is a mental disorder. It’s defined as an individual’s obsession
with the idea that some aspect of their appearance is severely flawed and
warrants exceptional measures to hide or rectify the offending part(s). In BDD's delusional variant, the flaw is
imagined and if some minor imperfection exists, its importance is severely
exaggerated. Sufferers find the symptoms
of BDD pervasive and intrusive, symptoms including excessive attention to the
perceived defect, social avoidance, camouflaging with cosmetics or apparel, the
seeking of verbal reassurances, avoiding mirrors, repetitively changing clothes
or restricting eating.
Italian physician Enrico Morselli (1852-1929)
in 1886 reported a disorder he termed dysmorphophobia, a term still sometimes
used in European literature to describe BDD.
Use spiked in academic literature in the 1950s although it wasn’t until
1980, the American Psychiatric Association (APA) recognized the condition in
the third edition of its Diagnostic and Statistical Manual of Mental Disorders
(DSM-III). The APA classified it as a
distinct somatoform condition (characterized by symptoms suggesting a physical
disorder but for which there are no demonstrable organic findings or known
physiological mechanisms) and in 1987 replaced dysmorphophobia with body
dysmorphic disorder as the preferred descriptor.
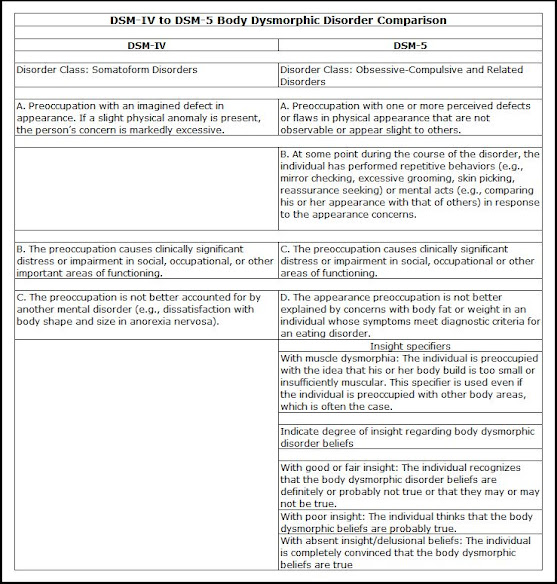
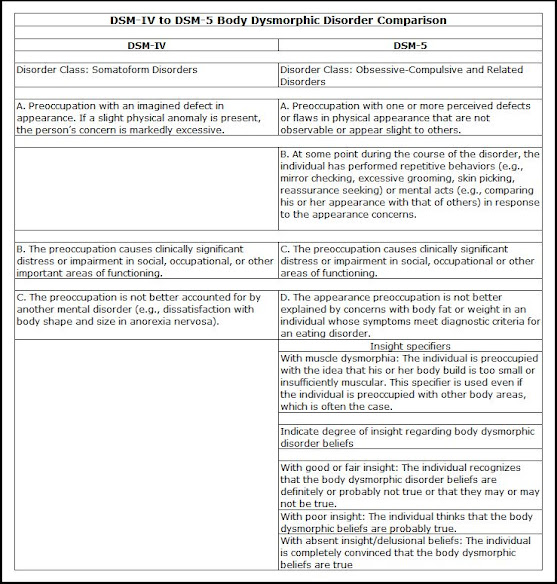
With the 1994 publication of DSM-IV, the
APA noted BDD was a preoccupation with an imagined or trivial defect in
appearance, one causing social or occupational dysfunction, and not better
explained as another disorder such as anorexia nervosa but in DSM-5 (2013), it
was reclassified as an obsessive-Compulsive and Related Disorder, adding
diagnostic criteria including repetitive behaviors and intrusive thoughts. Although the World Health Organization's (WHO) current International Classification of Diseases (ICD-10 (1994))
described BDD as just another hypochondriacal disorder, the revised ICD-11 (2019)
aligned for all functional purposes with the DSM-5.
The DSM-5 diagnostic criteria for BDD
requires the following:
(1) A preoccupation with appearance:
The individual must be preoccupied with one or more nonexistent or slight
defects or flaws in their physical appearance and “Preoccupation” is usually defined
as thinking about the perceived defects for (in aggregate) at least an hour a
day. A distressing or impairing
preoccupation with real and obvious flaws in appearance (anything easily
noticeable such as obesity) is not diagnosed as BDD, being instead classified
with “Other Specified Obsessive-Compulsive and Related Disorders.”
(2) Repetitive behaviors: Repetitive
and compulsive behaviors must manifest in response to the concern with appearance.
These compulsions can be behavioral and
thus observed by others (such as either excessively standing before or avoid a
looking-glass, frequent grooming, skin picking, reassurance seeking or repeatedly
changing clothes. Other BDD compulsions include
mental acts, the most often diagnosed being an individual frequently comparing their
appearance with that of other people. The
DSM-5 included the note for clinicians cautioning that subjects meeting all
diagnostic criteria for BDD except this one are not diagnosed with BDD; they
are diagnosed with “Other Specified Obsessive-Compulsive and Related Disorder.”
(3) Clinical significance: The
preoccupation must cause clinically significant distress or impairment in
social, occupational, or other important aspects of functioning. This criterion was included to differentiate
the disorder BDD, which requires treatment, from more normal appearance
concerns that typically do not need to be treated with medication or therapy. This has been one of the more controversial
revisions because of concerns it may exclude from helpful treatment some who
have developed better coping mechanisms while still suffering from the
underlying condition.
(4) Differentiation from an eating
disorder: If the appearance preoccupations focus on being too fat or
weighing too much, it may be that the appropriate diagnosis is an eating
disorder and this applies especially if the subject’s only concern with their
appearance focuses on excessive weight; provided the diagnostic criteria for an
eating disorder are otherwise met, that should be the diagnosis, not BDD. If not, BDD can be diagnosed, as concerns with
fat or weight in a person of normal weight can be a symptom of BDD and it’s not
uncommon for subjects to have both an eating disorder and BDD.
There are specifiers to BDD and following
diagnosis, the subject should be sub-classified using the two (DSM-5) BDD
specifiers:
(1) Muscle dysmorphia: Muscle dysmorphia is
the (predominately male) concern that the build of their body is too small or
insufficiently muscular, something which not untypically manifests with preoccupations
with other body areas; the muscle dysmorphia specifier should still be used in
such cases. Studies have shown that
among those diagnosed with BDD, those with muscle dysmorphia suffer the highest
rates of suicidality and substance use disorders, as well as poorer quality of
life. Accordingly, the DSM-5 notes their
treatment regimes may require some modification.
(2) Insight specifier: This
specifier indicates the degree (not directly frequency although this is a
factor in the analysis) of a subject’s insight regarding their BDD beliefs (eg “I
look ugly”; “I look deformed”), an expression of how convinced the subject is
that their beliefs about the appearance of the disliked body parts is true. The DSM-5 levels of insight are (2a) with good
or fair insight, (2b) with poor insight and (3), with absent insight/delusional
beliefs (which are to be diagnosed as BDD, not as a psychotic disorder.
BDD has often been misdiagnosed, most often
as one of the following disorders:
(1) Obsessive Compulsive Disorder:
If preoccupations and repetitive behaviors focus on appearance (including
symmetry concerns), BDD should be diagnosed rather than OCD.
(2) Social anxiety disorder (social
phobia): If social anxiety and social avoidance are due to embarrassment
and shame about perceived appearance flaws, and diagnostic criteria for BDD are
met, BDD should be diagnosed rather than social anxiety disorder (social
phobia).
(3) Major depressive disorder:
Unlike major depressive disorder, BDD is characterized by prominent
preoccupation and excessive repetitive behaviors. BDD should be diagnosed in
individuals with depression if diagnostic criteria for BDD are met.
(4) Trichotillomania (hair-pulling
disorder): When hair tweezing, plucking, pulling, or other types of hair
removal is intended to improve perceived defects in the appearance of body or
facial hair, BDD should be diagnosed rather than trichotillomania (hair-pulling
disorder).
(5) Excoriation (skin-picking disorder):
When skin picking is intended to improve perceived defects in the appearance of
one’s skin, BDD should be diagnosed rather than excoriation (skin-picking
disorder).
(6) Agoraphobia: Avoidance of
situations because of fears that others will see a person’s perceived
appearance defects should count toward a diagnosis of BDD rather than
agoraphobia.
(7) Generalized anxiety disorder:
Unlike generalized anxiety disorder, anxiety and worry in BDD focus on
perceived appearance flaws.
(8) Schizophrenia and schizoaffective
disorder: BDD-related psychotic symptoms (ie delusional beliefs about
appearance defects or BDD-related delusions of reference) reflect the presence
of BDD rather than a psychotic disorder.
(9) Olfactory reference syndrome:
Preoccupation with emitting a foul or unpleasant body odor is a symptom of
olfactory reference syndrome, not BDD (although these two disorders have many
similar characteristics).
(10) Eating disorder: If a
normal-weight person is excessively concerned about being fat or their weight,
meets other diagnostic criteria for BDD, and does not meet diagnostic criteria
for an eating disorder, then BDD should be diagnosed.
(11) Dysmorphic concern: This is not
a DSM diagnosis, but it is sometimes confused with BDD. It focuses on appearance concerns but also
includes concerns about body odor and non-appearance related somatic concerns,
which are not BDD symptoms.
One aspect of the condition BDD is that
it’s not uncommon for subjects to be reticent in revealing their concerns or BDD
symptoms to a clinician because of embarrassment or being negatively judged as vain
or too concerned with trivial matters.
Case notes do suggest there is a pattern of subjects hinting at their
issues and clinicians should thus be encouraged to respond by explicitly asking
about BDD symptoms.
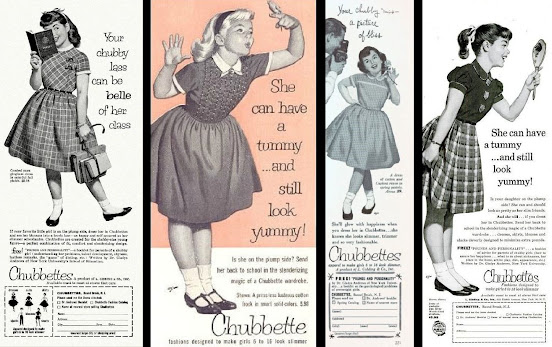
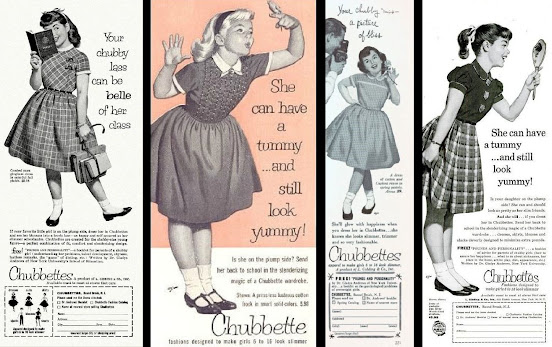
Although the brand-name is, strangely, no
longer used, in the late 1950s and early 1960s, Chubbettes was a fashion-house
supplying “slenderizing designs… designed
to make girls 6 to 16 look slimmer” and therefore become “as happy and self-assured as her slimmer
schoolmates”. With a target market
including those with eating disorders or BDD as well as the naturally chubby, Chubbettes
helpfully offered with its fashion catalog a free booklet, Pounds and Personality. Intended
for parents of a chubby girl and written by Dr Gladys Andrews of New York
University’s School of Education, it was packed with helpful hints about “understanding her problems, talent
development, shyness, tactless remarks & the “game” of dieting etc." Chubettes’ clothing range was said to be “available, coast to coast at stores that
care”; the parent company was L
Gidding & Co Inc, 520 Eighth Avenue, New York City.
Times certainly have changed and with them the perception of body shapes. Parents who would now regard young ladies of the type pictured in the Chubbette advertisements as being chubby might now be suspected of having Munchausen syndrome by proxy (MSbP). In the mind of the girl herself, a similar perception wouldn't necessarily alone be enough for a diagnosis of BDD but might be considered in the context of other behaviors.
Crooked Hillary Clinton, the Hamptons, August
2021.
Paradoxically, although in the early twenty-first century there’s a larger
than ever market for what Chubbettes once served as a niche, the brand is long
gone and a revival seems unlikely. Many
factors including more sedentary lifestyles and a higher consumption of
processed food, the sugar content of which has risen alarmingly, means demand
for more accommodating clothing will likely continue to increase but many
manufacturers have stepped into the Chubbette void and customers enjoy a wide
choice.