Dysmorphia (pronounced dis-mor-fiah)
(1) In clinical anatomy, characterized by anatomical malformation.
(2) In general medicine, having or exhibiting an anatomical malformation.
(3) In psychology and psychiatry, the perception of anatomical malformation; any of various psychological disorders whose sufferers believe that their body is wrong or inadequate, such as anorexia, bulimia, and muscle dysmorphia (bigorexia).
(4) As Dismorphia astyocha, a butterfly in the family Pieridae, found in both Argentina & Brazil.
From Ancient Greek δυσμορφίᾱ (dusmorphíā) (misshapenness, ugliness), the construct being δυσ- (dus-) (hard, difficult, bad) + μορφή (morphḗ) (shape, form) + -ίᾱ (-íā). The prefix dys- was from the New Latin dys-, from Ancient Greek δυσ- (dus-), (hard, difficult, bad”) and was used to convey the idea of being difficult, impaired, abnormal, or bad. Morph was a back-formation from morpheme & morphism, attested since the 1950s, from the Ancient Greek μορφή (morphḗ) (shape, form) and related to the German Morph, from Morphem (although dating only from the 1940s). It’s probably now most familiar in (1) formal grammar & linguistics as a physical form representing some morpheme in language (it exists as a recurrent distinctive sound or sequence of sounds), (2) in linguistics as an allomorph (one of a set of realizations that a morpheme can have in different contexts) and (3) in digital image processing where shapes are changed from one form to another with the use of specialized software, a popular type being that which wholly or (especially) partially blends two images. The plural is dysmorphias and, in clinical use, the synonym is dysmorphosis.
The word dysmorphia first appeared in the Histories of the Greek historian Herodotus (circa 484–circa 425 BC) when he referred to the myth of the “ugliest girl in Sparta”. Herodotus, even in his lifetime, was criticized for making an insufficient distinction between legend and historical fact but the veracity of much of his work, subject to forensic analysis by modern archeologists and archivists, has been established. The story of the “ugliest girl in Sparta” however, Herodotus acknowledges as “a magical myth” in which a baby girl, born in Sparta, was terribly disfigured (which he described as dysmorphia (meaning “misshapenness” or “ugliness”). Fortunately, she was from a well-connected family and her nanny suggested taking her to the shrine of Helen of Troy on hilltop of Therapne, and there pray for a cure. There the nurse sat with the baby and while praying before the agalma (a carved image of Helen), from nowhere a apparition of Helen appeared and smiling, laid her hand upon the child’s head. As the years passed, the disfigured infant would grow to become the most beautiful girl in the kingdom.
Body Dysmorphic Disorder
Body dysmorphic disorder (BDD) is a mental disorder. It’s defined as an individual’s obsession with the idea that some aspect of their appearance is severely flawed and warrants exceptional measures to hide or rectify the offending part(s). In BDD's delusional variant, the flaw is imagined and if some minor imperfection exists, its importance is severely exaggerated. Sufferers find the symptoms of BDD pervasive and intrusive, symptoms including excessive attention to the perceived defect, social avoidance, camouflaging with cosmetics or apparel, the seeking of verbal reassurances, avoiding mirrors, repetitively changing clothes or restricting eating.
Italian physician Enrico Morselli (1852-1929) in 1886 reported a disorder he termed dysmorphophobia, a term still sometimes used in European literature to describe BDD. Use spiked in academic literature in the 1950s although it wasn’t until 1980, the American Psychiatric Association (APA) recognized the condition in the third edition of its Diagnostic and Statistical Manual of Mental Disorders (DSM-III). The APA classified it as a distinct somatoform condition (characterized by symptoms suggesting a physical disorder but for which there are no demonstrable organic findings or known physiological mechanisms) and in 1987 replaced dysmorphophobia with body dysmorphic disorder as the preferred descriptor.
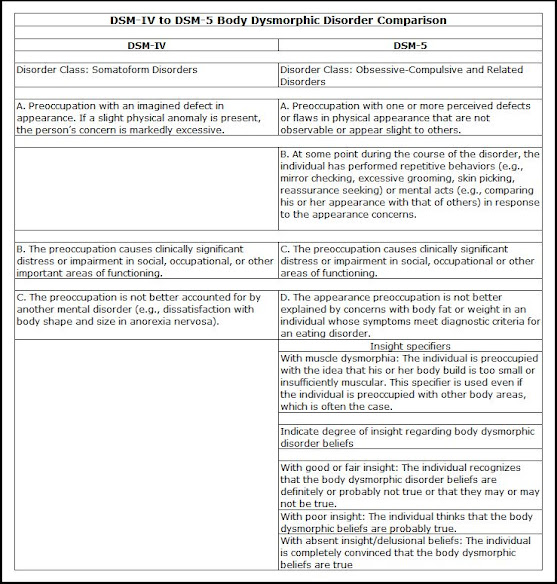
With the 1994 publication of DSM-IV, the APA noted BDD was a preoccupation with an imagined or trivial defect in appearance, one causing social or occupational dysfunction, and not better explained as another disorder such as anorexia nervosa but in DSM-5 (2013), it was reclassified as an obsessive-Compulsive and Related Disorder, adding diagnostic criteria including repetitive behaviors and intrusive thoughts. Although the World Health Organization's (WHO) current International Classification of Diseases (ICD-10 (1994)) described BDD as just another hypochondriacal disorder, the revised ICD-11 (2019) aligned for all functional purposes with the DSM-5.
The DSM-5 diagnostic criteria for BDD requires the following:
(1) A preoccupation with appearance: The individual must be preoccupied with one or more nonexistent or slight defects or flaws in their physical appearance and “Preoccupation” is usually defined as thinking about the perceived defects for (in aggregate) at least an hour a day. A distressing or impairing preoccupation with real and obvious flaws in appearance (anything easily noticeable such as obesity) is not diagnosed as BDD, being instead classified with “Other Specified Obsessive-Compulsive and Related Disorders.”
(2) Repetitive behaviors: Repetitive and compulsive behaviors must manifest in response to the concern with appearance. These compulsions can be behavioral and thus observed by others (such as either excessively standing before or avoid a looking-glass, frequent grooming, skin picking, reassurance seeking or repeatedly changing clothes. Other BDD compulsions include mental acts, the most often diagnosed being an individual frequently comparing their appearance with that of other people. The DSM-5 included the note for clinicians cautioning that subjects meeting all diagnostic criteria for BDD except this one are not diagnosed with BDD; they are diagnosed with “Other Specified Obsessive-Compulsive and Related Disorder.”
(3) Clinical significance: The preoccupation must cause clinically significant distress or impairment in social, occupational, or other important aspects of functioning. This criterion was included to differentiate the disorder BDD, which requires treatment, from more normal appearance concerns that typically do not need to be treated with medication or therapy. This has been one of the more controversial revisions because of concerns it may exclude from helpful treatment some who have developed better coping mechanisms while still suffering from the underlying condition.
(4) Differentiation from an eating disorder: If the appearance preoccupations focus on being too fat or weighing too much, it may be that the appropriate diagnosis is an eating disorder and this applies especially if the subject’s only concern with their appearance focuses on excessive weight; provided the diagnostic criteria for an eating disorder are otherwise met, that should be the diagnosis, not BDD. If not, BDD can be diagnosed, as concerns with fat or weight in a person of normal weight can be a symptom of BDD and it’s not uncommon for subjects to have both an eating disorder and BDD.
There are specifiers to BDD and following diagnosis, the subject should be sub-classified using the two (DSM-5) BDD specifiers:
(1) Muscle dysmorphia: Muscle dysmorphia is the (predominately male) concern that the build of their body is too small or insufficiently muscular, something which not untypically manifests with preoccupations with other body areas; the muscle dysmorphia specifier should still be used in such cases. Studies have shown that among those diagnosed with BDD, those with muscle dysmorphia suffer the highest rates of suicidality and substance use disorders, as well as poorer quality of life. Accordingly, the DSM-5 notes their treatment regimes may require some modification.
(2) Insight specifier: This specifier indicates the degree (not directly frequency although this is a factor in the analysis) of a subject’s insight regarding their BDD beliefs (eg “I look ugly”; “I look deformed”), an expression of how convinced the subject is that their beliefs about the appearance of the disliked body parts is true. The DSM-5 levels of insight are (2a) with good or fair insight, (2b) with poor insight and (3), with absent insight/delusional beliefs (which are to be diagnosed as BDD, not as a psychotic disorder.
BDD has often been misdiagnosed, most often as one of the following disorders:
(1) Obsessive Compulsive Disorder: If preoccupations and repetitive behaviors focus on appearance (including symmetry concerns), BDD should be diagnosed rather than OCD.
(2) Social anxiety disorder (social phobia): If social anxiety and social avoidance are due to embarrassment and shame about perceived appearance flaws, and diagnostic criteria for BDD are met, BDD should be diagnosed rather than social anxiety disorder (social phobia).
(3) Major depressive disorder: Unlike major depressive disorder, BDD is characterized by prominent preoccupation and excessive repetitive behaviors. BDD should be diagnosed in individuals with depression if diagnostic criteria for BDD are met.
(4) Trichotillomania (hair-pulling disorder): When hair tweezing, plucking, pulling, or other types of hair removal is intended to improve perceived defects in the appearance of body or facial hair, BDD should be diagnosed rather than trichotillomania (hair-pulling disorder).
(5) Excoriation (skin-picking disorder): When skin picking is intended to improve perceived defects in the appearance of one’s skin, BDD should be diagnosed rather than excoriation (skin-picking disorder).
(6) Agoraphobia: Avoidance of situations because of fears that others will see a person’s perceived appearance defects should count toward a diagnosis of BDD rather than agoraphobia.
(7) Generalized anxiety disorder: Unlike generalized anxiety disorder, anxiety and worry in BDD focus on perceived appearance flaws.
(8) Schizophrenia and schizoaffective disorder: BDD-related psychotic symptoms (ie delusional beliefs about appearance defects or BDD-related delusions of reference) reflect the presence of BDD rather than a psychotic disorder.
(9) Olfactory reference syndrome: Preoccupation with emitting a foul or unpleasant body odor is a symptom of olfactory reference syndrome, not BDD (although these two disorders have many similar characteristics).
(10) Eating disorder: If a normal-weight person is excessively concerned about being fat or their weight, meets other diagnostic criteria for BDD, and does not meet diagnostic criteria for an eating disorder, then BDD should be diagnosed.
(11) Dysmorphic concern: This is not a DSM diagnosis, but it is sometimes confused with BDD. It focuses on appearance concerns but also includes concerns about body odor and non-appearance related somatic concerns, which are not BDD symptoms.
One aspect of the condition BDD is that it’s not uncommon for subjects to be reticent in revealing their concerns or BDD symptoms to a clinician because of embarrassment or being negatively judged as vain or too concerned with trivial matters. Case notes do suggest there is a pattern of subjects hinting at their issues and clinicians should thus be encouraged to respond by explicitly asking about BDD symptoms.
Although the brand-name is, strangely, no longer used, in the late 1950s and early 1960s, Chubbettes was a fashion-house supplying “slenderizing designs… designed to make girls 6 to 16 look slimmer” and therefore become “as happy and self-assured as her slimmer schoolmates”. With a target market including those with eating disorders or BDD as well as the naturally chubby, Chubbettes helpfully offered with its fashion catalog a free booklet, Pounds and Personality. Intended for parents of a chubby girl and written by Dr Gladys Andrews of New York University’s School of Education, it was packed with helpful hints about “understanding her problems, talent development, shyness, tactless remarks & the “game” of dieting etc." Chubettes’ clothing range was said to be “available, coast to coast at stores that care”; the parent company was L Gidding & Co Inc, 520 Eighth Avenue, New York City.
Times certainly have changed and with them the perception of body shapes. Parents who would now regard young ladies of the type pictured in the Chubbette advertisements as being chubby might now be suspected of having Munchausen syndrome by proxy (MSbP). In the mind of the girl herself, a similar perception wouldn't necessarily alone be enough for a diagnosis of BDD but might be considered in the context of other behaviors.
Paradoxically, although in the early twenty-first century there’s a larger than ever market for what Chubbettes once served as a niche, the brand is long gone and a revival seems unlikely. Many factors including more sedentary lifestyles and a higher consumption of processed food, the sugar content of which has risen alarmingly, means demand for more accommodating clothing will likely continue to increase but many manufacturers have stepped into the Chubbette void and customers enjoy a wide choice.


No comments:
Post a Comment